It’s a great time to be a microbe. Gone are the days of being cast as a pathogenic pest to be eradicated with antibiotics. “Good bacteria” are all the rage. Every day there’s a new article cheerfully reporting the latest (often tenuous) link between human health and the trillions of microorganisms housed by our bodies. Amidst the enthusiasm over the human microbiome there is also a resurgence in interest in probiotics – live microorganisms consumed for their purported health benefits. Not everyone is thrilled about how these products are being sold and advertised. In his book “Missing Microbes,” Martin Blaser spends over 200 pages detailing the many ways in which he believes damage to the human microbiome caused by antibiotics and the like are harming our health, yet he draws the line at recommending probiotics, calling the largely unregulated industry “the Wild West.” I tend to feel the same way. I recently chastised a friend for taking acidophilus, arguing that there was no good evidence to support its use. But then I realized I’d been saying the same thing for some years now without ever checking to see if the research situation had improved. Science, especially that surrounding health, is a work in progress. Perhaps probiotics deserve a second look.
Probiotics and gut health
We may as well start in the gut, since that’s where your yogurt and probiotic pills are heading. Earlier this summer, the International Scientific Association for Probiotics and Prebiotics (ISAPP) published their expert panel recommendations on the use of the word “probiotics” and the health claims made about these products. Their slightly updated (tweaked for grammar) definition of probiotics states they are, “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host.” The panel also came to the surprising agreement that for certain well-studied probiotic species* some general claims about health benefits could be made. I say surprising because everything else I’ve read has stressed the importance of not generalizing a clinical benefit shown in one microbial species, or even one strain, to the whole lot (i.e., just because Lactobacillus rhamnosus fixed your tummy ache doesn’t mean L. acidophilus could do the same). What are these general benefits you ask? They’re vague concepts like, “supporting a healthy gut microbiota” and “supporting a healthy digestive tract.”
Personally, I’m underwhelmed by the word “supporting.” Supporting what functions exactly, and how? Part of the problem with making sense of the research on probiotics is that, when they do seem to work, their mechanisms of action are not fully understood. The probiotic pills you buy at the health food store may claim they work by restoring your “natural balance” of good bacteria, but crowding out harmful microbes is only one possible means by which probiotics accomplish their ends. Other mechanisms include strengthening the intestinal barrier and producing antimicrobial compounds that kill pathogens, as well as compounds that can affect the immune system. And different strains likely employ different mechanisms, or combinations of mechanisms.
Additionally, there isn’t some archetypal perfect microbiome out there, nor are we entirely sure yet what a healthy one looks like. The ISAPP readily acknowledges this, stating that, “the current state of science does not allow the clear definition of a healthy gut microbiota based on microbial composition.” So the idea that a single probiotic or even a particular mixture of probiotics would be beneficial for all humans is a bit premature.
Much of the ISAPP document feels like a compromise struck between science and industry. But for potential consumers of probiotics, only the science is of interest. And what of the science? Does research show that these products actually work? Well, yes and no. The research certainly doesn’t say that all probiotics are useless. But evidence of their efficacy is hard to sort out. Different studies use different species or strains of probiotics against different gastrointestinal ailments, and, unfortunately, all this research isn’t organized into a user friendly matrix connecting each of the microbes to each of the maladies with a 4-star rating system to indicate relative success or failure.
Looking at meta-studies (studies of studies) offers some hope in clarifying matters. A 2012 paper published in PLoS One examined randomized controlled trials conducted on 11 probiotic species to treat or prevent various gastrointestinal illnesses. They found all but three species to be effective, though in varying degrees, for six of the ailments (including irritable bowel syndrome and antibiotic-associated diarrhea), while no significant effect was seen for traveler’s diarrhea or necrotizing enterocolitis (though other studies have reported contrary findings on the latter).
But this approach comes with it’s own set of drawbacks. For instance, some microbes are just studied more than others, which can affect how their performance looks in a meta-analysis. And while the PLoS One study provides support for the idea general benefits (eight of eleven probiotics were at least somewhat effective), the variation in probiotic performance suggests that matching the microbe to the malady would be preferable to just picking one at random.
Still, the relationship between probiotics and digestive health is probably the most established, least contentious of their potential effects. Let’s pause for a moment to appreciate this semblance of confidence, because from here we move into murkier waters…
Probiotics and the immune system
“Boosts your immune system!” “Supports your healthy immune system!” So say the probiotic supplement packages, but what does that even mean? Apparently, not a lot. The ISAPP panel, after being so generous about gut health claims, decided that such statements were too vague to be included among the probiotic core benefits.
The immune system is all kinds of complicated. When it’s weakened, the body is more susceptible to infection. Yet an overachieving immune system can result in allergies and autoimmune diseases. Sure, there’s evidence that our bodies’ microbes play a role in immune function, but we don’t yet know enough about what they do or how they do it to be able to employ probiotics as a tool.
The research on probiotics and immune disorders is nowhere near coalescing into a clear picture of cause and effect. For example, while studies have found that patients with eczema (a skin disease that may be caused in part by immune system malfunction) have different gut microbe composition than those without, a 2008 review on treatment of eczema with probiotics concluded that there was not sufficient evidence to recommend using them.
Attempting to treat serious immune disorders with probiotics alone is obviously not a good idea. But there’s another potential target demographic of the “supports your immune system” claim: essentially healthy people who want to be even healthier. Which probiotic(s) should they take? Any immune system effects of probiotics are likely species or strain specific. Some microbes have anti-inflammatory properties while others are pro-inflammatory. If you aren’t trying to solve a particular problem, how do you choose one probiotic over another? And how would you assess whether or not your product was working? It’s a lot of guesswork for something than can cost as much as 30 dollars for a month’s worth of pills.
Probiotics and weight
Weight management is one of those areas where science is easily overshadowed by wishful thinking. Wouldn’t it be nice if all one needed to go from fat to thin was a microbiome adjustment, courtesy of probiotics? It’s not unreasonable to think that microbes could affect weight. After all, gut bacteria do help us digest food and extract calories. On top of that, research has found some differences in the microbiomes of obese versus non-obese individuals (though again, we don’t know if it’s causal). And at least one strain of bacteria – Lactobacillus gasseri SBT2055 – has been linked to weight loss. This might be a good time to recall that we can’t necessarily generalize properties of one probiotic strain to all probiotics. To wit, some species have been linked to weight gain. It has even been suggested that probiotics might contribute to obesity. Though this is a disputed claim, in part because weight gain is not always a bad thing. Patients who suffer from chronic diarrhea may be struggling to absorb enough calories from their food. If probiotics resolve that ailment, you would expect to see some weight gain. So, once again, it’s complicated.
In any event, there’s no reason to believe that probiotics are going to singlehandedly fix our growing obesity problem. And even in studies with more radical alterations of gut microbiota (caveat: in mice, not humans) diet was still a factor.
Probiotics for the ladies
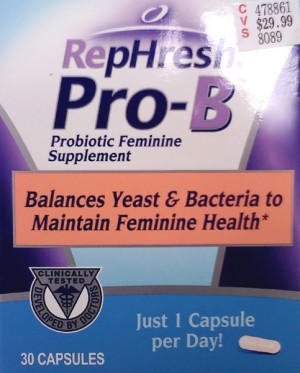
For many women, the first encounter with the concept of probiotics is as a folk remedy for yeast infections. I was a little surprised that the probiotic supplements I found in the store weren’t touting this potential application along with their other non-FDA-evaluated claims. But then I realized there was a whole separate section of probiotics for women with promises of “supports vaginal health” or, if you prefer, the more euphemistic “supports feminine health.”
While anecdotes abound on this topic, the research is still a little thin. On the bright side, there aren’t quite as many species of microbes to choose from. Bacteria of the genus Lactobacillus dominate the vaginal microbiota, so those are the logical ones to try. Most studies of probiotics to treat vulvovaginal candidiasis (yeast infection) or bacterial vaginosis (another common problem often self-misdiagnosed as yeast infection) use Lactobacilli in addition to standard therapies, so there’s little to report on whether probiotics alone are of any use. As adjunct therapies, they showed some promise in reducing symptoms and infection relapses, but more research is needed before any recommendations can be made.
What could possibly go wrong?
While there are plenty of reasons to be skeptical of probiotic’s efficacy, at least we can agree that they’re harmless, right? Well, mostly. Nothing you put into your mouth, including food, water, and your own fingers is 100% safe. And, while probiotics are generally low on side-effects, you might want to be aware of bacteremia – a potentially fatal complication in which bacteria find their way into the blood, which can result in septic shock. Don’t freak out, it’s quite rare. A study in Finland, where use of the probiotic Lactobacillus rhamnosus GG rose precipitously after it became available in 1990, found no increase in bacteremia. However, it’s a risk worth considering for certain susceptible populations, namely anyone with a compromised immune system and premature infants.**

For the general population though, the biggest threat probiotics pose is to the wallet. There is currently no evidence to support long-term probiotic use by healthy people, yet the probiotic section of supplement aisle seems stocked to provide every man, woman, and child with a lifetime supply of these things. It’s pretty likely that many folks are taking probiotics to no avail.
However, I will concede that there is some promise for using probiotics to treat or prevent specific maladies – particularly in the area of gastrointestinal disease. It doesn’t seem absurd to take probiotics to potentially lessen the damage of a round of antibiotics. And you probably won’t be laughed out of your doctor’s office for asking if swallowing microbes might improve IBS. A note about dose: that “when administered in adequate amounts” bit means at least 1 billion organisms. Not every product with the word “probiotic” on its label (including yogurt) contains that quantity of microbes, so if you’re going to buy this stuff do at least read the fine print.
Overall, probiotics are not an established treatment option so much as a just-in-case approach. Benefits may be species specific, strain specific, or even host specific (i.e., just because it worked for your friend doesn’t mean it will work for you). And there isn’t enough research yet to customize your microbial therapy, so you’re on your own in terms of picking a product. If I’d been on the ISAPP panel I’d have suggested ditching “supports a healthy gut microbiota” for something more realistic like, “this might help, but then again it might not” or perhaps “uncertainty is the only certainty there is.”
* The lucky microbes the ISAPP felt worth including are Bifidobacterium (species: adolescentis, animalis, bifidum, breve and longum) and Lactobacillus (species: acidophilus, casei, fermentum, gasseri, johnsonii, paracasei, plantarum, rhamnosus and salivarius).
** Unfortunately, premature infants are also the main victims of necrotizing enterocolitis – a life-threatening condition that causes tissue death in the bowel – for which probiotic therapy may be useful.











