
Updated April 2, 2020:
The US just became the first country to have more than thousand COVID19 deaths within one day. https://t.co/FsLvwmrmPK
— Florian Krammer (@florian_krammer) April 2, 2020
#COVID19 update April 01 global:
935,022 cases, 47,189 deaths, 193,989 recovered
U.S. 26,000+ cases and 1,000+ deaths today
big increases in Spain, Germany, France, Italy, U.K.
Canada 9,730 cases, 111 deaths#globalhealth pic.twitter.com/23HJXZfvaY— André Picard (@picardonhealth) April 2, 2020
The grim story for the US death curve on April 1st is that it has crossed Italy's, steeply heading to Spain. Not a hint of improvement; >500 deaths/day now
New York's slope is still worst in the world.https://t.co/568QRBEJ6s pic.twitter.com/CukPH8DN3v— Eric Topol (@EricTopol) April 1, 2020
1. The U.S. Centers for Disease Control and Prevention (CDC) is considering advising people to use masks in public. The New York Times reports that as many as 25% of infected people may not show symptoms but could still spread the SARS-CoV-2 virus that causes COVID-19. This may explain why the virus has spread so rapidly.
Early data suggests many who are infected are not symptomatic, which is why we are recommending you use cloth face coverings plus physical distancing for essential activities.
Do not use surgical and N95 masks, which are reserved for first responders and medical workers.
— MayorOfLA (@MayorOfLA) April 2, 2020
The decision to wear a mask depends on each person’s unique situation. For some help in figuring out what you should do, please check out these two articles, one by Tara Haelle at Forbes and the other by The Atlantic’s Ed Yong.
Should Everyone Wear A Mask In Public? Maybe—But It’s Complicated via @forbes
-Good read ???https://t.co/P60f2wQSUw— ??? ? ??????, ??? ?????? (@MackayIM) April 2, 2020
On masks, many ppl have Very Strong Opinions. I don't think it's clear-cut either way, and I've tried to lay out & evaluate the reasons for/against widespread usage. I hope it's useful to ppl making hard decisions amid contradictory views & imperfect datahttps://t.co/UbmISGQYDN
— Ed Yong (@edyong209) April 1, 2020
2. In Iceland, 1% of people in a sample of 9,000 from the general population tested positive for COVID-19. However, of that 1%, about half of those people did not show symptoms or had mild symptoms at the time of testing. This finding, reported by CNN, confirms other studies that the virus is likely being spread by asymptomatic people.
Iceland lab's testing suggests 50% of coronavirus cases have no symptomshttps://t.co/6gBhbOj4Oh
— Dr. Joseph Fair (@curefinder) April 1, 2020
3. In the U.S., hospitals in hard hit areas continue to experience severe shortages of personal protective equipment (PPE).
In the 27 mins since posting this, I’ve received dozens of messages from healthcare workers all over the country. AZ, CA, LA, MI, TX…
Exact same situation. Masks are rationed. Can’t speak up. Not good for ‘hospital optics’.
OUR FRONLTINE PROVIDERS WILL DIE.
WE NEED PPE! https://t.co/JI6EIKF1va
— Craig Spencer MD MPH (@Craig_A_Spencer) April 2, 2020
Protective gear in national stockpile is nearly depleted, DHS officials say https://t.co/74vhG4tksH
— Carl Zimmer (@carlzimmer) April 1, 2020
Unfortunately, a new critical shortage is looming: medications. Esther Choo, a physician and health policy expert, warned about it in a Twitter thread:
It’s clear from speaking with peers around the country that we’re running into shortages of medications like fentanyl, versed, propofol, and paralytic. Why these particular medications? And why do we care? A #WeNeedMeds thread. 1/
— Esther “STAY HOME” Choo, MD MPH (@choo_ek) April 1, 2020
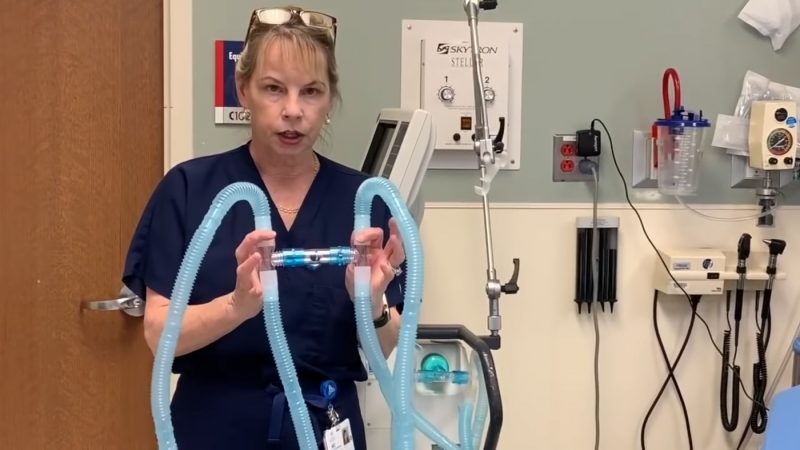
When a patient is placed on a ventilator, they need to be sedated because a rigid tube is inserted down the throat, called intubation. This painful procedure requires medications that are in very short supply. Stat News recently wrote about this imminent problem.
On top of the overwhelming shortages of medical equipment to combat Covid-19, medicines needed for patients placed on ventilators are also in short supply. https://t.co/pc1Sx3PIJ8
— STAT (@statnews) March 31, 2020
4. At locations in the U.S. hardest hit by COVID-19 cases, healthcare workers are being forced to do their jobs with very limited PPE, placing them at higher risk of infection. That’s causing increasing fear and anxiety among the doctors, nurses, respiratory therapists, nurse’s aides, and other staff who look after patients.
I lost my mother (also a physician) when I was 19.
I’ve never been scared to go to work until now.
I just want to be here for my babies and to see them grow up.— uché blackstock (@uche_blackstock) March 30, 2020
Just like our ERs & ICUs, our EMS colleagues are reaching a breaking point. They’re worried about their supply of personal protective equipment. They’re worried about more calls & sicker patients, in crowded apartments. Seeing the sad reality on the frontlines, they’re afraid…
— Craig Spencer MD MPH (@Craig_A_Spencer) March 29, 2020
On March 31, the first U.S. emergency room physician died from COVID-19.
I lost my best friend to Covid19 a few hours ago. ?@DrFrankGabrin? was an ER Doctor in NYC. He planned to go back to work when he recovered. It took only five days from the first sign of symptoms. He leaves a husband of less than one year behind. We are devastated. #PPENow pic.twitter.com/LVOSe9XXG6
— Debra Vasalech Lyons (@DebVasalech) March 31, 2020
Dr. Frank Gabrin had been treating coronavirus patients on the front lines. He died in his husband’s arms just days after showing symptoms.
His heartbroken husband honors his memory tonight on the show as a hero “who loved to help people." pic.twitter.com/SKAHH9txlt
— Cuomo Prime Time (@CuomoPrimeTime) April 2, 2020
Bill Fisher, an ER doctor and former astronaut, is 74 years old, diabetic, and has blood type A. Most of these factors put him at a high risk group for COVID-19.
I’m a full-time ER doc getting ready to work a 24 hour shift in the emergency department. I am genuinely more concerned about going to work tomorrow morning than I was the day I launched on the space shuttle. 1.5% shuttle mortality vs 9-12% if I get COVID-19.
— Dr. Bill Fisher (@DrBillFisher) April 1, 2020
The situation is so dire that some healthcare workers are updating their advanced directives.
I reviewed my existing advance directive w/ my loved ones this weekend. Sobering? Difficult? Yes. Also a necessity for every adult in these times & ALL times. It’s never too early to prepare for emergencies and crises #AdvanceCarePlanningProtectsYourWisheshttps://t.co/DPcP4gB9Ox
— Sandy Tun, MD (@SandyTunMD) March 29, 2020
I’m a young ER doctor and today I reviewed my Last Will & Testament. Times like these are an opportunity for us all to embrace vulnerability and prepare as best we can for whatever the future may hold. pic.twitter.com/Be3wURaZUG
— David Zodda, MD (@DavidZodda) March 31, 2020
Some healthcare workers, afraid to infect their families, have temporarily moved out of their homes.
Just said bye to my wife, leaving her with her parents so I can work without worrying that I’m compromising her health and safety by doing my job. I’m just one of many in this boat, not knowing when we will see our loved ones again. This virus sucks. #COVID19 #medtwitter
— Stephen C. Dorner, MD, MPH, MSc (@StephenDorner) April 1, 2020
With two young boys, a wife and elderly mother-in-law at home, this emergency room physician knew that if he wasn't cautious, he could spread the novel coronavirus to his own family. Now, thanks to a Facebook group, he's got one less thing to worry about. https://t.co/wM9VRGYNU1
— KITV4 (@KITV4) April 2, 2020
I miss my kids. But we are all in the right place.
Tomorrow I am getting an apt, so I can go back to the ER and they can come home. https://t.co/4cbnNaQvyT
— Dara Kass, MD (@darakass) March 28, 2020
There have been several cases of doctors and nurses being fired for speaking out about the lack of PPE that puts them at extreme risk of infection.
Doctors and nurses are the superheroes of our day. My new column looks at how hospitals are punishing and sometimes firing them for speaking up about inadequate personal protective equipment. This is where the unconscionable meets the idiotic: https://t.co/8Bwmh9WKO9
— Nicholas Kristof (@NickKristof) April 1, 2020
And it’s been physically and emotionally draining ….
After a week on #COVID19 service, I have some non-clinical reflections for #hospitalists. This is NOT your regular ward time. I’ll be honest, it was a tough week. I’ll start with the tough stuff. But stick with me – ending with more positivity and some helpful hints.
— Leora Horwitz (@leorahorwitzmd) March 31, 2020
Last night in the ICU of a #NYC hospital, I cared for 20 patients who were all on breathing machines due to #COVID19. Some REALLY young (20s), without comorbidities. Everyone is extremely sick. But sicker patients keep flooding in…
— Prakriti Gaba (@PrakritiGaba) March 29, 2020
Comfort dog lending support to an emergency room doctor during COVID-19 crisis. pic.twitter.com/5ZwgcxaiDD
— Lorenzo The Cat (@LorenzoTheCat) March 29, 2020
5. The SARS-CoV-2 virus arrived in Africa, after gaining a foothold in Asia, Europe, and North America, when a case was reported in Nigeria at the end of February.
#COVID19 – SURVEILLANCE UPDATE: 1 APRIL 2020 – 5:00 pm EAT
African Union Member States (49) reporting COVID-19 cases (5,940), deaths (210), and recoveries (426) by region.
More information on >>> https://t.co/fvcEaCHn37#COVID19 #FactsNotFear #AfricaPrepares #AfricaResponds pic.twitter.com/XOHTE2uReV— Africa CDC (@AfricaCDC) April 1, 2020
In a March 31 article posted at Berkeley News, University of California Berkeley economist Edward Miguel, an expert in African economics, expressed concern about what lies ahead:
Even though health infrastructure has improved, in some ways, it remains severely deficient. Most sub-Saharan African countries have very few beds in hospital intensive care units. Some articles I’ve read say Kenya has only 155 ICU beds – for a country of 50 million people.
That’s terrifying. If there’s a significant outbreak, even if there aren’t as many vulnerable elderly people, millions of people still could be affected. Very few will have the care they need with ventilators and other advanced treatment.
Africa is a very diverse continent, with some countries better equipped to handle the pandemic than others. You can read more about these complexities in an extended interview at the Berkeley News website.
6. A “cytokine storm” is when your immune system goes into overdrive, even after the virus has been largely destroyed, attacking vital organs. Doctors think that this happens for as many as 15% of seriously ill patients, and may explain why some young people die from COVID-19. An article in the New York Times explains how it works.
Why do some younger patients get hit so hard by coronavirus? A "cytokine storm" from their own immune systems might be the reason. https://t.co/n0FVTwFPQe
— NYT Science (@NYTScience) April 2, 2020
7. Anthony Fauci, director of the U.S. National Institute of Allergy and Infectious Diseases, has become a household name for many Americans, a trusted source for medical and epidemiological information about COVID-19. As a result of increasing threats and other unwelcome attention, he has been assigned a security detail.
Exclusive: Anthony Fauci, the face of the U.S. response to the coronavirus pandemic, is facing growing threats to his personal safety, prompting the government to step up his security https://t.co/l5fgKlgwQA
— The Washington Post (@washingtonpost) April 2, 2020
Updated April 1, 2020:
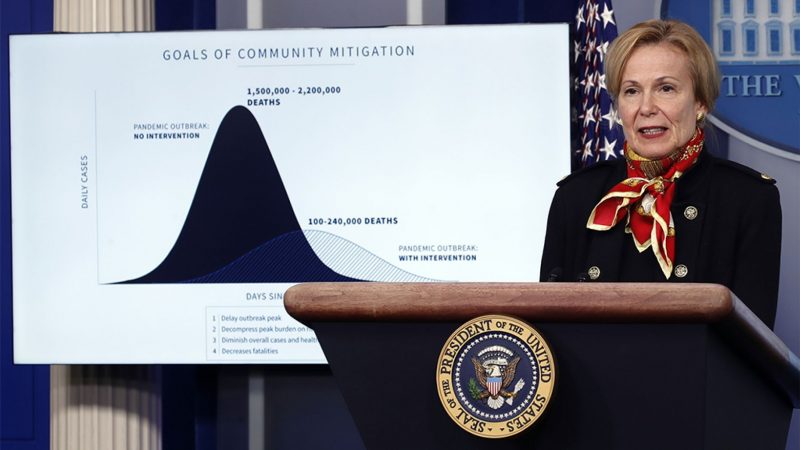
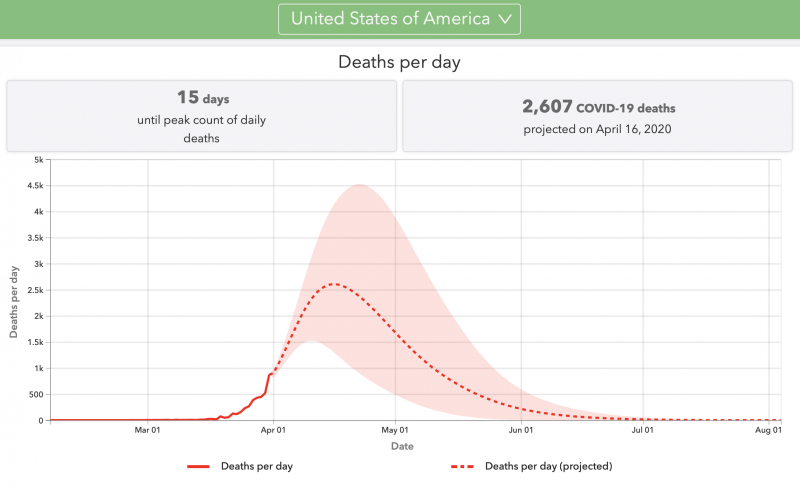
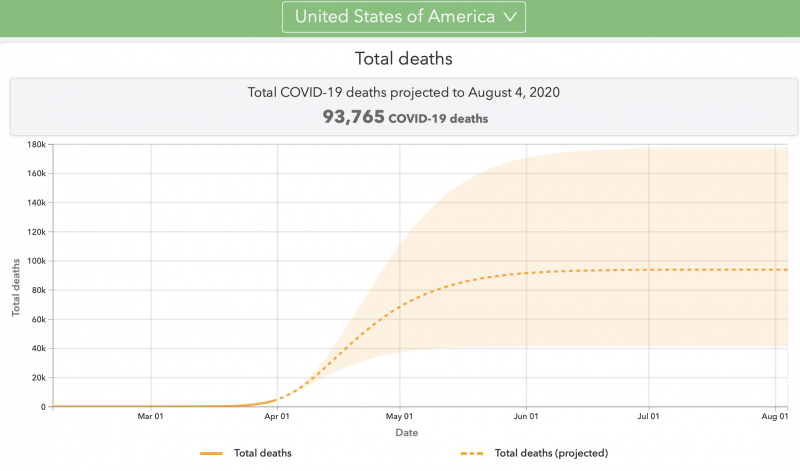
Just one quick update today, a brief look at the announcement from the White House late yesterday about new modeling work from the University of Washington, which provides new projections for the COVID-19 infection and death rate in the U.S. Assuming the strictest of lockdowns feasible in this country, there could still be 100,000 to 240,000 deaths in this country. Without these precautions, the number of deaths could be 1.5 to 2.2 million in the U.S. There is an associated website with much good information. You can see U.S. state-by-state projections, and much more. We’ll have more on how physicians and scientists are reacting to this new model soon.
Note that these numbers are not predictions (they’re not conclusions deduced from a given set of facts). Scientists don’t tend to predict. Instead, they project (arrive at a numeric conclusion, based on calculations and numbers, in a way that’s quantitative and analytical). In a way similar to projections about changes to Earth’s climate over the coming century, the numbers are not set in stone. They are subject to change as conditions change, and as scientists (now rushing to understand COVID-19 and its effects on our world) continue to ply their trades of mathematics, physics, computing and more.


Updated March 30, 2020:
As of Sunday (March 29) evening, there are 141,995 confirmed COVID-19 cases in the U.S., of which at least 2,486 people have lost their lives. For updates, try this excellent New York Times article tracking the pandemic in the U.S. and around the world. For more international news, try the World Health Organization’s Situation Report page. You might also check the U.S. Centers for Disease Control and Prevention cases and updates page. And another good one is Johns Hopkins’ interactive map page. And Worldometers offers this page.
1. At a White House press conference on Sunday, March 29, President Trump extended social distancing guidelines until April 30. Originally, the federal guidelines suggested March 30 as an ending date.
The Associated Press wrote:
President Donald Trump on Sunday extended the country’s voluntary national shutdown for a month, significantly changing his tone on the coronavirus pandemic only days after musing about the country reopening in a few weeks. He heeded public-health experts who told him the virus could claim over 100,000 lives in the U.S., perhaps more, if not enough is done to fight it.
COVID-19 continues its relentless spread, as the daily number of infections worldwide continues to jump sharply. World Health Organization figures show the increase in new infections is now about 70,000 per day – up from about 50,000 just days ago. More than 32,000 people have died worldwide. The U.S. had over 139,000 infections and 2,400 deaths, a running tally by a prominent university showed Sunday evening.
2. In a Twitter post, Tom Inglesby (@T_Inglesby), director of Johns Hopkins Center for Health Security, explained why the administration made the right call about extending the social distancing guidelines period. Social distancing continues to be the best way to reduce transmission of the SARS-CoV-2 virus (coronavirus); without these precautions, hospitals would be unable to cope with the very large numbers of sick people. He warned that places with low incidents of COVID-19 should use this time to prepare for the inevitable increase in sick people.
(Note: the Twitter boxes you see here are links to the original tweet on Twitter. Click inside the box to open the post in Twitter. Some tweets are “threads:” consecutive tweets by one author and/or with responses from others. To see all that – and that’s where the meat is – click on the link on this page, then click again once you’re inside Twitter. Try looking for the words “show this thread.”)
The Administration today made the important right decision to extend social distancing guidelines. Its worth underscoring why those measures are so critical, and considering the conditions in which they might be able to be relaxed safely sometime in the future. 1/x
— Tom Inglesby (@T_Inglesby) March 30, 2020
Inglesby also drew attention to a report, published on the American Enterprise Institute website, on how, going forward, the country should deal with the pandemic and what’s needed to bring the spread under control.
A very well done report addressing conditions needed for relaxing social distancing came out today called: National Coronavirus Response: A Roadmap to Re-opening. https://t.co/G8d8zT8C78 written by @ScottGottliebMD @CMYMAMark M McClellan, L Silvis, @C_R_Watson 12/x
— Tom Inglesby (@T_Inglesby) March 30, 2020
3. The critical shortage of personal protective equipment (PPE) continues. In an op-ed for The Hill, emergency room doctor Craig Spencer made yet another compelling case for immediately using the Defense Production Act to produce more PPEs – masks, gowns, and eye protection – and other life-saving equipment. He wrote:
My colleagues on the frontline fighting coronavirus are facing a drastic shortage of personal protective equipment (PPE).
To protect them – the doctors, nurses and other health care providers treating critical patients every hour of every day – the federal government must immediately mobilize the Defense Production Act and the Strategic National Stockpile.
Yesterday the president ordered General Motors to make ventilators under the Act. He must do the same for PPE. Only by ordering U.S. industries to increase the supply of PPE will we ensure all health care workers have access to the tools we need to stay safe during this pandemic. Otherwise many of us – myself included – are at exceptionally high risk of being exposed and infected.
Pictured here is a Frontline Coronavirus Nurse in a Greater Boston Hospital treating her COVID-19 patients in a RAINCOAT after running out of medical gowns. This Nurse happens to be my wife. The PPE shortage is real. DO YOUR JOB AND STAY HOME ? #Covid_19 #HealthcareHeroes pic.twitter.com/fvHGbHrXjA
— Angela Santa Fe (@CoachA_SantaFe) March 28, 2020
4. Some US healthcare workers have been posting about their experiences on Twitter. Here are some of them.
Dear Environmental Services,
There are a million images of heroic doctors & nurses, but you are the ones fighting to keep us safe. Scrubbing halls & walls & disinfecting every surface—without the benefit of know who touched it before you. You are heroes. I celebrate you. #COVID19— Stephanie Graff, MD, FACP (@DrSGraff) March 29, 2020
Last night in the ICU of a #NYC hospital, I cared for 20 patients who were all on breathing machines due to #COVID19. Some REALLY young (20s), without comorbidities. Everyone is extremely sick. But sicker patients keep flooding in…
— Prakriti Gaba (@PrakritiGaba) March 29, 2020
I am an emergency medicine doctor.
I don't "have" patients.
Most of the time, I care for patients and never see them again. #COVID19 has changed that.
1/
— Dara Kass, MD (@darakass) March 29, 2020
Today.
I told a 28 year old that he needs intubation. He was scared. Couldn’t breathe.
I told the wife of a 47 year old that he is dying over FaceTime.
I bronched a #COVID19 patient who mucous plugged. It saved his life. Risked mine.
— Anna Podolanczuk (@AnnaPodolanczuk) March 29, 2020
Saw this photo floating around and couldn't find the source. Happy to say it's, in fact, real. Was taken by a ramp agent.
Pictured are about 30 nurses from Atlanta-area hospitals headed to NYC to help with covid-19 efforts.https://t.co/fEPqHitaEH pic.twitter.com/Pl6z4UsrjM
— Jane Lytvynenko ??????????????? (@JaneLytv) March 29, 2020
Here’s a post from Ian Haydon, who volunteered for a vaccine trial. Thank you, Ian, and thank you to all who are volunteering to help as we continue along the uncharted road of the COVID-19 pandemic of 2020.
I've been admitted into the 1st COVID-19 vaccine trial.
I'm grateful for my health. For the 1000s of scientists who brought us here. For the team that developed this vaccine (@NIH, @moderna_tx, et al). For @KPWaResearch, and the nurse who came out of retirement to draw my blood pic.twitter.com/phxai5wsYZ
— ian haydon (@ichaydon) March 28, 2020
Updated March 28, 2020:
Editors’ Note: The U.S. now leads the world with the most confirmed COVID-19 cases: 101,819, of which there are 1,619 deaths (as of Friday evening). If more testing was available, the number of confirmed cases would be greatly higher. Within the U.S. population of 330 million people, there is an urgent need to severely reduce the spread of COVID-19 now. So far, because we’re in a crisis situation, many of the studies suggesting treatments have had small sample sizes and/or are being published online without peer review. Scientists are working furiously to understand whether any of these medications have the looked-for outcome in treating the disease; so far, the verdict isn’t in.
1. There are several COVID-19 hotspots around the country. New York City has almost half the known number of COVID-19 cases in the U.S. Other hotspots are emerging in cities such as Detroit, Chicago and New Orleans. The New York Times is tracking cases, and has a country-wide map showing the distribution of COVID-19 cases.
I’m worried about emerging situations in New Orleans, Dallas, Atlanta, Miami, Detroit, Chicago, Philadelphia, among others. In China no province outside Hubei ever had more than 1,500 cases. In U.S. 11 states already hit that total. Our epidemic is likely to be national in scope. pic.twitter.com/jfN6YYRT07
— Scott Gottlieb, MD (@ScottGottliebMD) March 27, 2020
One of my books was titled I HEARD THE SIRENS SCREAM about 9/11 & anthrax. As bad as that was, the steady 24/7 wailing of ambulance sirens in NYC these #COVID19 days is relentless. I find myself reflexively running to the windows when one gets close by.https://t.co/gYz2VWVvpk
— Laurie Garrett (@Laurie_Garrett) March 27, 2020
The worst is likely yet to come for New Orleans in the fight against coronavirus, according to the U.S. Surgeon General.
MORE: https://t.co/rQkKkcIEqT
"We see places like Detroit, like Chicago and like New Orleans that are due for a New York-type week next week."
— NOLA.com (@NOLAnews) March 28, 2020
The Army Corps of Engineers is working to convert Chicago’s McCormick Place convention center into a 3,000-bed hospital for coronavirus patients, an official says. https://t.co/GxywguR8bi
— Chicago Tribune (@chicagotribune) March 28, 2020
"Confirmed cases in Los Angeles County rose by more than 50% in a single day, reaching 1,200." California faces perilous two weeks as coronavirus cases, deaths surge. https://t.co/4UTbgWflUQ #COVID19
— Deborah Blum (@deborahblum) March 27, 2020
2. There are still not enough COVID-19 tests in the U.S. for all who request them. The situation is improving with each passing day, but slowly. The COVID-19 Tracking Project is compiling most results from labs around the country.
Our daily update is published. We've now tracked 626,667 completed tests, with more than ~100k reported over the last 24 hours.
Note: We think we are capturing roughly 90% of tests completed.
For state-by-state details, see: https://t.co/PZrmH4bl5Y pic.twitter.com/M2K5sM2i43
— The COVID Tracking Project (@COVID19Tracking) March 27, 2020
Bloomberg News reports that Abbott Laboratories was just granted FDA approval to distribute a new test – one that looks for fragments of the SARS-CoV-2 virus – that delivers results in minutes, as opposed to other tests that can take as long as a few days. The first batch of 50,000 tests will be distributed on April 1.
Note that there are two kinds of tests:
(i) to find out if a person is infected, a test is needed to detect the presence of the SARS-CoV-2 virus. Those tests are critically needed at hospitals, and have been severely hampered by delays.
(ii) the other test detects the presence of antibodies specific to the virus. When a person is infected, the body mounts a defense against the virus, creating antibodies that specifically destroy the virus. This test is useful to find out how many people have already been infected and are immune to the virus; remember, not everyone who was infected had symptoms. It cannot be used to find out if a patient is currently infected because the body has not had enough time to create these antibodies.
3. There has been a widespread misconception that young people are immune to COVID-19. While most acute cases are seen in older people and people with a compromised immune system, there have been some serious cases involving young healthy people. An article in The Atlantic starkly illustrates this point.
"The fact is that young people with no clear underlying health conditions are getting seriously ill from COVID-19 in significant numbers. And young Americans—no matter how healthy and invincible they feel—need to understand that." – Kerry Meltzer, NYC doc https://t.co/NZNiFer38z
— Ed Yong (@edyong209) March 26, 2020
The author, Kerry Kennedy Meltzer, a doctor in New York City, wrote:
I am 28 years old. Up until Friday, when people asked me whether I was scared, I would tell them yes – for my country, my colleagues, my 92-year-old grandmother, and all the people most vulnerable to getting seriously ill from the virus, but not for myself. I, like many others, believed that young people were less likely to get sick, and that if they did, the illness was mild, with a quick recovery.
I now know that isn’t the case. The fact is that young people with no clear underlying health conditions are getting seriously ill from COVID-19 in significant numbers. And young Americans – no matter how healthy and invincible they feel – need to understand that.
Here’s a twitter post about a young couple who contracted the virus.
I was mildly sick for a few days w/ covid symptoms. Then my 29 yr old healthy boyfriend got really sick. 13 days later, after a relentless fever, awful nausea, pneumonia in both lungs + a reluctant trip to ER, he is finally turning a corner today. Some things I learned:
— Eliza Shapiro (@elizashapiro) March 26, 2020
4. The Washington Post reports a continued shortage of personal protective equipment (PPE). Doctors are reusing masks after disinfecting them, which is not normal practice and may not adequately protect them against droplets in the air carrying the virus. The CDC has issued guidelines for reusing masks, but it is not an ideal solution. People across the country are stepping up to gather supplies via local appeals from hospitals and local governments to large-scale coordinations by organizations like Project N95. There are also campaigns, like #MasksNow, to sew masks. If you want to donate homemade masks directly to your local hospital, please contact them first to find out if they’re accepted for use.
.@umichmedicine is asking the community to donate gear to protect health care workers and patients from #COVID19.
Drop-off donation site open daily starting Saturday, March 21 at the North Campus Research Complex, at corner of Huron Pkwy and Plymouth Rdhttps://t.co/Gv2YOcm5ql pic.twitter.com/obmAELzWXE
— Michigan Medicine (@umichmedicine) March 20, 2020
Some progress is being made in getting more PPEs and ventilators but hospitals and state governments say they are hampered by having to bid against each other for these vital supplies.
5. Ventilators are used to do the work of breathing for critically ill COVID-19 patients by pushing air into their lungs. At this stage, patients have already developed severe pneumonia: the lungs have become inflamed and the patient struggles to breathe as fluid accumulates in air sacs in the lungs. In an article in The Guardian, Christine Jenkins, of Lung Foundation Australia, said:
Unfortunately, so far we don’t have anything that can stop people getting Covid-19 pneumonia.
People are already trialing all sorts of medications and we’re hopeful that we might discover that there are various combinations of viral and anti-viral medications that could be effective. At the moment there isn’t any established treatment apart from supportive treatment, which is what we give people in intensive care.
We ventilate them and maintain high oxygen levels until their lungs are able to function in a normal way again as they recover.
And there is an acute shortage of these life-saving ventilators in the U.S. One doctor has come up with a “hack” to connect two patients to a single ventilator. At least one hospital in New York City has had to resort to it. This is not an ideal solution because machines are set by the amount of air pressure pumped into the lungs, and different patients may need different pressure settings. But in desperate times …
We wrote about this extreme measure, which hasn't been tested in humans, a week ago. It's now being used in New York-Presbyterian Hospital https://t.co/6MV9ga47Gn
— Emanuel Eggberg (@emanuelmaiberg) March 26, 2020
‘The Other Option Is Death’: New York Starts Sharing of Ventilators https://t.co/a6bTiqQ4WI
— Carl Zimmer (@carlzimmer) March 27, 2020
Some doctors have also found that they get better results by having patients lie on their stomach for oxygen therapy and ventilator support.
Still splitting ventilators and proning patients. This is just EXPERIMENTAL. No evidence, just doing things out of necessity. Difficult to track the results. Ping @khaycock2 @ThinkingCC @PulmCrit @emcrit @iceman_ex pic.twitter.com/PbqQNaVOLz
— marco garrone (@drmarcogarrone) March 27, 2020
This tweet explains why having patients lie on their stomach helps them get more oxygen. Turn up the volume to hear it more clearly.
Families and folk who've seen it on the news are asking me why we ventilate their loved ones on their tummies… so here, in 75 seconds, and slightly simplified, is why! #COVID2019 pic.twitter.com/xxPQl4Daza
— Dr. Ron Daniels BEM (@SepsisUK) March 26, 2020
On a grim note, hospitals are also preparing for the possibility that they will have to triage severely ill patients, making excruciating decisions about who lives and who dies. An internal memo was circulated to medical staff at the Henry Ford Health System in Michigan with instructions on how to decide, among the critically ill, who should be treated in the event of a shortage of ventilators. The hospital confirmed the memo was authentic but said it was a worst case scenario, and they had not arrived at that point. This is a situation that all besieged hospitals will have to confront if there are not enough ventilators for those patients who need it.
Henry ford hospital Michigan. Mother in-law works here and it is this bad! Thoughts and prayers. Please stay safe. pic.twitter.com/xYGjnxL0ux
— grayson gray (@graysongray9) March 27, 2020
As your trusted healthcare provider, our duty is to be prepared for worst case scenarios. Yesterday you may have seen an internal policy that has been circulated but not yet implemented. Here is our response: pic.twitter.com/W1orpUUJ5t
— Henry Ford News (@HenryFordNews) March 27, 2020
6. What is the path going forward? If you haven’t already, please read an outstanding article by Ed Yong in The Atlantic titled How the Pandemic will End.
For the immediate future, the University of Washington has created a tool that helps states predict the course of outbreaks so they can plan ahead.
this tool made by the University of Washington projects when the covid outbreak will peak in each state and how bad it'll get. in California, it will peak April 24, when 148 people die in a single day https://t.co/j2Shn7kICo
— Soumya (@skarlamangla) March 27, 2020
Scott Gottlieb, former FDA commissioner and a fellow at the American Enterprise Institute, wrote a Twitter thread about what it will take to reduce this outbreak in the coming months.
THREAD: Our path to safety rests on massive support for our healthcare system to care for sick, and forceful steps by local leaders to break chains of transmission and quell epidemic spread. If we’re smart and aggressive across nation, cases nationally could peak by late April.
— Scott Gottlieb, MD (@ScottGottliebMD) March 27, 2020
7. For a quick roundup of Friday’s political news of the day, try this article from The Hill: 16 things to know today about the coronavirus outbreak. It includes the fact that the House passed, and President Trump signed, the $2 trillion coronavirus stimulus legislation, the largest emergency spending bill in U.S. history. It reports that Trump also invoked the Defense Production Act for the first time, to make General Motors manufacture respirators. But, according to The Hill:
… we don’t know how many respirators the administration needs, or how many they want from GM.
The Hill also reports on more states enacting quarantines or outright travel bans, and on the fact that the coronavirus is inexorably making its way through the U.S. Congress.

Updated March 27, 2020:
Breaking news:
From the BBC: U.K. Prime Minister Boris Johnson tests positive for coronavirus
Here are some links to basic information you might need, as we plow forward through the ongoing coronavirus pandemic.
World Health Organization’s coronavirus entry page
World Health Organization’s coronavirus “myth-busters” page
The U.S. Centers for Disease Control and Prevention (CDC) coronavirus entry page
New York Times‘ coronavirus entry page (all coverage free during the pandemic)
Washington Post’s coronavirus live updates page (all coverage free during the pandemic)
The Hill’s 15 things to know today about coronavirus (from March 26)
Plus:
From RocketCityMom, a video: This doctor shows us how to sanitize groceries, and it’s very useful (and terrifying)
From the Washington Post: Why not to panic about shopping, getting delivery or accepting packages
Last but not least:
From the European Space Agency: Coronavirus lockdown leading to drop in pollution across Europe

Updated March 26, 2020:
1. British science journalist Ed Yong has written a compelling piece in The Atlantic on the COVID-19 outbreak in the U.S.: where the response went wrong and what we may see in the coming months. The article, released on March 25, is an excellent read. It’s called How the Pandemic Will End.
?I wrote a big piece about the future of the COVID-19 pandemic: how the US got to this point; what needs to happen in the coming weeks and months; what the endgame looks like; and what the world might be like in the aftermath. https://t.co/woc4dxwT0Z
— Ed Yong (@edyong209) March 25, 2020
Yong described the severity of this unprecedented pandemic:
Having fallen behind, it will be difficult – but not impossible – for the United States to catch up. To an extent, the near-term future is set because COVID-19 is a slow and long illness. People who were infected several days ago will only start showing symptoms now, even if they isolated themselves in the meantime. Some of those people will enter intensive-care units in early April. As of last weekend, the nation had 17,000 confirmed cases, but the actual number was probably somewhere between 60,000 and 245,000. Numbers are now starting to rise exponentially: As of Wednesday morning, the official case count was 54,000, and the actual case count is unknown. Health-care workers are already seeing worrying signs: dwindling equipment, growing numbers of patients, and doctors and nurses who are themselves becoming infected.
Italy and Spain offer grim warnings about the future. Hospitals are out of room, supplies, and staff. Unable to treat or save everyone, doctors have been forced into the unthinkable: rationing care to patients who are most likely to survive, while letting others die. The U.S. has fewer hospital beds per capita than Italy. A study released by a team at Imperial College London concluded that if the pandemic is left unchecked, those beds will all be full by late April. By the end of June, for every available critical-care bed, there will be roughly 15 COVID-19 patients in need of one. By the end of the summer, the pandemic will have directly killed 2.2 million Americans, notwithstanding those who will indirectly die as hospitals are unable to care for the usual slew of heart attacks, strokes, and car accidents. This is the worst-case scenario. To avert it, four things need to happen – and quickly.
The first thing, Yong said, was addressing the alarming shortage of basic emergency room supplies such as masks, gloves, and other equipment that protects health care workers.
The second is widespread testing; Yong explained why initial efforts failed, and how the situation is improving as the FDA has been quickly granting approvals for tests from private labs.
Thirdly, he wrote about the critical importance of social distancing to slow the spread of the virus, to keep hospitals from being overwhelmed with patients.
And his fourth point: efforts to slow the spread of the virus requires clear coordination. To date, the federal government has not issued clear guidelines. Some state and local governments, on the advice of epidemiologists, have taken matters into their own hands while other states have not adopted these mitigation strategies.
Slowing down the pace of the outbreak isn’t enough. As long as the virus is out there, it will continue to infect people. Yong described three possible scenarios for how it could play out. The best approach, he wrote, is to stamp out outbreaks until there’s a vaccine.
Labs around the world are already working on a vaccine. This is a long process that requires extensive testing for safety; it could take 12 to 18 months, and even longer to mass produce. Until then, periods of social distancing may be needed to keep the disease spread at manageable levels for health care workers. How this plays out, Yong says, will depend on several factors, including seasonal effects on virus transmission, how long immunity lasts for people who were infected, development of antiviral drugs, and close monitoring and suppression of outbreaks.
Yong also laid out the sobering realities of the painful economic, psychological, and health care impacts on society as the U.S. battles the COVID-19 outbreak. However, this experience could also bring about positive social changes such as new ways of working, fairer labor policies, and a better health care system.
Ed Yong’s article in The Atlantic is thoughtful, thorough, and thought-provoking. We highly recommend you read it in its entirety.
2. New York City, the largest and most densely-populated city in the U.S., is already being hit hard in the initial stage of the COVID-19 pandemic. The New York Times reports, as of the evening of March 25, there were over 20,000 confirmed cases and 280 deaths. City-wide, over 3,922 people have been hospitalized with COVID-19.
One article described the distressing situation at the Elmhurst Hospital Center in Queens. Over a 24-hour period, they lost 13 patients.
People have died in the ER while waiting for a bed. There aren't enough ventilators. This entire hospital will soon be dedicated to the coronavirus.
New York City hospitals are at the center of the pandemic in the U.S. “It’s apocalyptic," one doctor said. https://t.co/f6kJU33yI7
— The New York Times (@nytimes) March 25, 2020
They reported 199 total deaths in NYC at 10am. By 6pm, it was 280 deaths. That's 81 deaths in 8 hours, or a death every 6 minutes.
— George Takei (@GeorgeTakei) March 26, 2020
3. An article in Nature describes how the blood of patients who recovered from COVID-19, who have antibodies against the SARS-CoV-2 virus, will be used as an experimental therapy in New York City hospitals.
Hospitals in New York City are gearing up to use the blood of people who have recovered from #COVID19 as a possible antidote for the disease. It follows preliminary studies in China that attempted the measure with plasma from people who had recovered. https://t.co/RlZHsqDOrt
— Nature (@nature) March 25, 2020
4. At the March 25 White House briefing, Anthony Fauci, who leads the National Institute of Allergy and Infectious Diseases, suggested that COVID-19 could be a seasonal disease. As the Southern Hemisphere moves towards the colder season, more cases are appearing there. Fauci is quoted in an article in The Hill as saying:
I know we’ll be successful in putting this down now, but we really need to be prepared for another cycle.
5. Health policymakers depend on mathematical models to guide their plans for protecting the public against disease outbreaks. But in situations where there’s not enough information about a pathogen, like the SARS-CoV-2 virus, modeling disease outcomes in a population can be tricky.
This is described in a brief overview in The Guardian:
This is quite possibly the best general news reporting I've seen on mathematical modeling in years. Bravo https://t.co/bqhRzopkRl
— Bill Hanage (@BillHanage) March 26, 2020
There’s a more detailed account in Science:
Computer models have never been more important in the response to an infectious disease. That puts a huge responsibility on the modelers. New story by @kakape and me: https://t.co/QzXKaDi1rB
— Martin Enserink (@martinenserink) March 25, 2020
6. In states where governments have shut down businesses and encouraged people to work from home, a new appreciation is emerging for the people who keep our society functioning. Economist Byron Auguste tweeted this on March 22:
Restaurant staff, grocery clerks, health aides, sanitation workers, etc., are low-wage—not low-skill.
They do quality control, optimize time tradeoffs, navigate social-emotional dynamics.
And in the midst of #COVID19, they are making major sacrifices to keep our society afloat.
— Byron Auguste (@byron_auguste) March 22, 2020
Updated March 24, 2020:
1. A day in the life of ER doctor Craig Spencer, in New York City.
Thank you everyone for your incredible messages of support and encouragement.??
Many of you asked what it was like in the ER right now. I want to share a bit with you. Please RT:
A Day in the Life of an ER Doc – A Brief Dispatch from the #COVID19 Frontline:
— Craig Spencer MD MPH (@Craig_A_Spencer) March 24, 2020
2. New York Times journalist Donald G. McNeil Jr. has written a fascinating article about what it will take to get through the COVID-19 outbreak. He interviewed experts and studied what was done in China, South Korea, Singapore, and Taiwan, where efforts to beat back the outbreak have, so far, yielded promising results.
McNeil interviewed David L. Heymann of the World Health Organization. Heymann noted that the virus infects clusters of people within families, friends, and work colleagues. He told McNeil:
You can contain clusters. You need to identify and stop discrete outbreaks, and then do rigorous contact tracing.
In talking to experts in contagious diseases, McNeil found that they all agreed on the steps that need to be taken. He wrote:
Americans must be persuaded to stay home, they said, and a system put in place to isolate the infected and care for them outside the home. Travel restrictions should be extended, they said; productions of masks and ventilators must be accelerated, and testing problems must be resolved.
3. Some policy wonks, politicians, and media pundits have suggested that stay-at-home orders instituted by some state governors are too extreme and will severely hurt the economy. They think people should return to work at the end of the federal government’s 15-day social distancing period. This take captured the interest of President Trump who tweeted about it on March 22:
WE CANNOT LET THE CURE BE WORSE THAN THE PROBLEM ITSELF. AT THE END OF THE 15 DAY PERIOD, WE WILL MAKE A DECISION AS TO WHICH WAY WE WANT TO GO!
— Donald J. Trump (@realDonaldTrump) March 23, 2020
The Hill reported on March 23 that Trump and his advisors are having fierce debates about how long coronavirus restrictions should stay in place. The Hill wrote:
A number of people around Trump have pushed for prioritizing the economy and sending people back to work as quickly as possible, particularly in less afflicted areas. But Trump’s own public health officials and some of his allies on Capitol Hill have warned against risking higher infection rates and deaths for the sake of boosting the economy in the short term.
Public health experts and scientists continue to say that – given what we know to date – only social distancing and/or a vaccine can contain the COVID-19 pandemic. They say the consequences of ending the coronavirus restrictions too early would be devastating to the elderly and people with underlying health conditions. Tom Inglesby, of the Johns Hopkins School of Public Health, said in a tweet:
Many models report that health care systems will be completely overwhelmed/collapse by the peak of cases if major social distancing is not put in place …
COVID would spread widely, rapidly, terribly, could kill potentially millions in the yr ahead with huge social and economic impact across the country.
4. The anti-malarial drugs chloroquine and hydroxychloroquine have made the news in recent days as a potential treatment for COVID-19. Public health experts are cautioning that there’s not yet enough evidence for this claim and are concerned about side effects that could be harmful. Interest in this drug originated from a French study with a small sample size (number of patients) where the drug was found to improve symptoms.
Clinical trials for hydroxychloroquine have started or will be starting at research institutions in the U.S. and the World Health Organization. Some doctors are also using it — in the absence of other treatments — on their severely ill patients.
Recent interest in this drug, especially President Trump’s enthusiasm for it, has already led to shortages. This is causing considerable hardships for lupus and rheumatoid arthritis patients who use it to modulate an overactive autoimmune system. Some people have taken matters into their own hands with tragic consequences; in Phoenix, Arizona, a man died after consuming chloroquine phosphate, a chemical used to treat parasites in aquarium fish. His wife was in critical condition.
For additional details about hydroxychloroquine and chloroquine, please see the New York Times article about it.
Toxicologist here.
Chloroquine and hydroxychloroquine are not yet proven to treat or prevent #COVID19. They may have a role; we just don’t know yet.
Too much (or from drug interactions) can cause hypotension, hypokalemia, seizures, and fatal cardiac dysrhythmias. 1/3
— Bryan D Hayes PharmD (@PharmERToxGuy) March 23, 2020
5. Former FDA commissioner Scott Gottlieb says even though most people who succumb to COVID-19 are ages 60 years and older, young people can fall seriously ill and suffer long-term effects from their illness.
While vast majority of deaths from #COVID19 are age 60+ many young adults and middle aged Americans are becoming seriously ill and surviving only after prolonged hospitalizations and ICU admissions that have long term consequences. This is a dangerous virus for most age groups. pic.twitter.com/jVYWFatTDM
— Scott Gottlieb, MD (@ScottGottliebMD) March 23, 2020
Note: this table is from a CDC report.
6. The numbers we see in the news – of the dead, the sick – represent real people, each with family, friends, and community that cherishes them. Here is one story.
I need to share a #COVID19 letter from Rome. The writer is on the Board of an intl school there.
She writes:
"This is an account of what my family and I are going through now – this instant. I'm a private person. I don't share photos or family stories on social media…"
MORE pic.twitter.com/Mqumb7OorN— Laurie Garrett (@Laurie_Garrett) March 24, 2020
7. The numbers we are seeing, however, are likely not the entire story. They represent only confirmed cases, that is, only cases involving positive tests for COVID-19. In the U.S. last week, testing was not widely available. A new batch of tests was released a few days ago, but, to date, not everyone who requests a test for the disease can get a test, plus some people may choose never to ask for a test. You see that – if everyone in the U.S. were tested for COVID-19 simultaneously – we could identify and isolate those with the disease and the pandemic (in this country) would be over. However, as things stand, there are unreported cases of the disease in the U.S. population.
Another case in point is Russia, which – as of March 23, 2020 – was reporting fewer than 500 cases of COVID-19. A story in EuroNews reported:
President Vladimir Putin had told Russians last week that timely measures put into place at the onset of the outbreak had helped to avoid a ‘massive epidemic’ in the country. Putin had insisted that, in the largest country on the planet, coronavirus infections are ‘under control.’ As of Monday, out of the world’s more than 350,000 confirmed cases, only 438 have been reported in Russia … Suspicions are rife that the official figures could be false, because the data coming out of Russia seems to be contradictory. The Rosstat statistical agency claims pneumonia cases in Moscow increased by 37% in January 2020 compared to 2019.
Bottom line: EarthSky’s essential coronavirus links from March 24 to April 6, 2020. A roundup of information from physicians, scientists and journalists about the COVID-19 pandemic.











